Sterilization Methods and their Relation to Beyond-Use Dates in the New USP <797>
James Zellner, ARL Bio Pharma Technical Sales
In the upcoming version of USP <797> Pharmaceutical Compounding – Sterile Preparations, the method of sterilization has a significant impact on the maximum allowable Beyond-Use date (BUD) a compounded preparation may be assigned. The two approaches to sterilization in the chapter are aseptic processing and terminal sterilization. Terminal sterilization provides the longest BUDs possible but may not be compatible with the compounded preparation due to the conditions required to sterilize. Ultimately, the appropriate sterilization method for a particular formulation depends on the product, with the allowable BUD a consequence.
The new version of USP <797> equates the maximum allowable BUD with the method of sterilization. USP defines terminal sterilization as the “application of a lethal process (e.g., steam, dray heat, irradiation) to sealed containers for the purpose of achieving a predetermined PNSU (Probability of Non-Sterile Unit) of greater than 10-6 or a probability of less than one in a million of a nonsterile unit”. Aseptic processing is defined as “a method by which separate, sterile components are brought together under conditions that maintain their sterility. The components can either be purchased as sterile or, when starting with nonsterile components, can be separately sterilized prior to combining.” Tables in the chapter are presented for Category 2 and Category 3 products that state the conditions that must be met to assign a particular BUD.
Table 1. BUD Limits for Category 2 CSPs – Assuming a Sterility Test has Been Performed and Passed
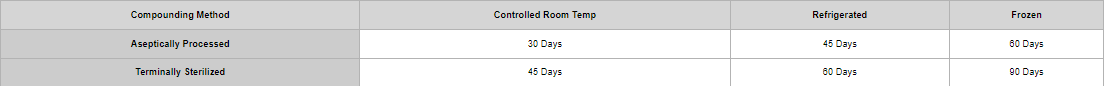
Table 2. BUD Limits for Category 3 CSPs – Assuming a Sterility Test has Been Performed and Passed
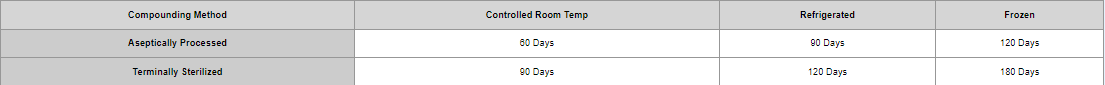
Based on the tables above, the maximum BUD allowed in USP <797> is 180 days if the product is terminally sterilized and stored frozen. BUDs are reduced from this maximum based on the storage conditions and sterilization method. Terminal sterilization is given a preferential BUD since a sterility assurance level can be reliably calculated and the variable risk of contamination during compounding is eliminated since a sealed, finished product is sterilized at the very end of the process. Of note, USP does not consider filter sterilization a Terminal Sterilization method. Aseptic processing, without a final, sealed container sterilization step, requires aseptic conditions be maintained throughout the process to deliver a sterile finished product. When choosing or changing a sterilization method for a preparation, a BUD study utilizing a validated, stability indicating method is necessary. If BUD data was previously demonstrated using aseptic processing, and the pharmacy wants to now utilize terminal sterilization, the BUD study must be repeated to demonstrate the product meets all test criteria.
The tolerance of the product, in conjunction with the tolerance of the container system, dictate whether a particular formulation may be terminally sterilized. Temperature-sensitive preparations may be impossible to sterilize terminally, given the typical temperatures and times required (121o C for 15 minutes or more). Container systems may degrade under terminal sterilization conditions. When considering the use of terminal sterilization, the whole formulation must be taken into account. Even if the active pharmaceutical ingredient is stable, excipients, to include any preservatives, may break down, rendering them inert for the intended purpose. If terminally sterilized, USP requires those products made from nonsterile ingredients, or compounded using nonsterile devices, be sterilized within 6 hours of compounding. This is to minimize the generation of bacterial endotoxins. Logistical and scheduling issues may occur depending on the number of product lots made, container sizes, and throughput of the terminal sterilization process. USP also requires terminal sterilization specific measures be taken for SOPs and validation of the sterilization cycle. SOPs specifying the temperature, duration, load conditions, and biological indicator use must be written. Training and competency of personal on the terminal sterilization process must be recorded and kept. Utilizing terminal sterilization requires an in- depth knowledge of the product, logistical considerations, thorough SOPs, and continuous monitoring of the effectiveness of the procedure to properly implement.
A compounded sterile preparation’s BUD is derived from numerous factors. One of the most important being the method used to achieve a sterile finished product. Terminal sterilization and aseptic processing both have advantages and disadvantages which must be thoroughly examined to decide which is best for each product.
References:
· USP <797>